ULTRASOUND SYSTEM AND METHOD FOR ACQUISITION PARAMETER DETERMINATION
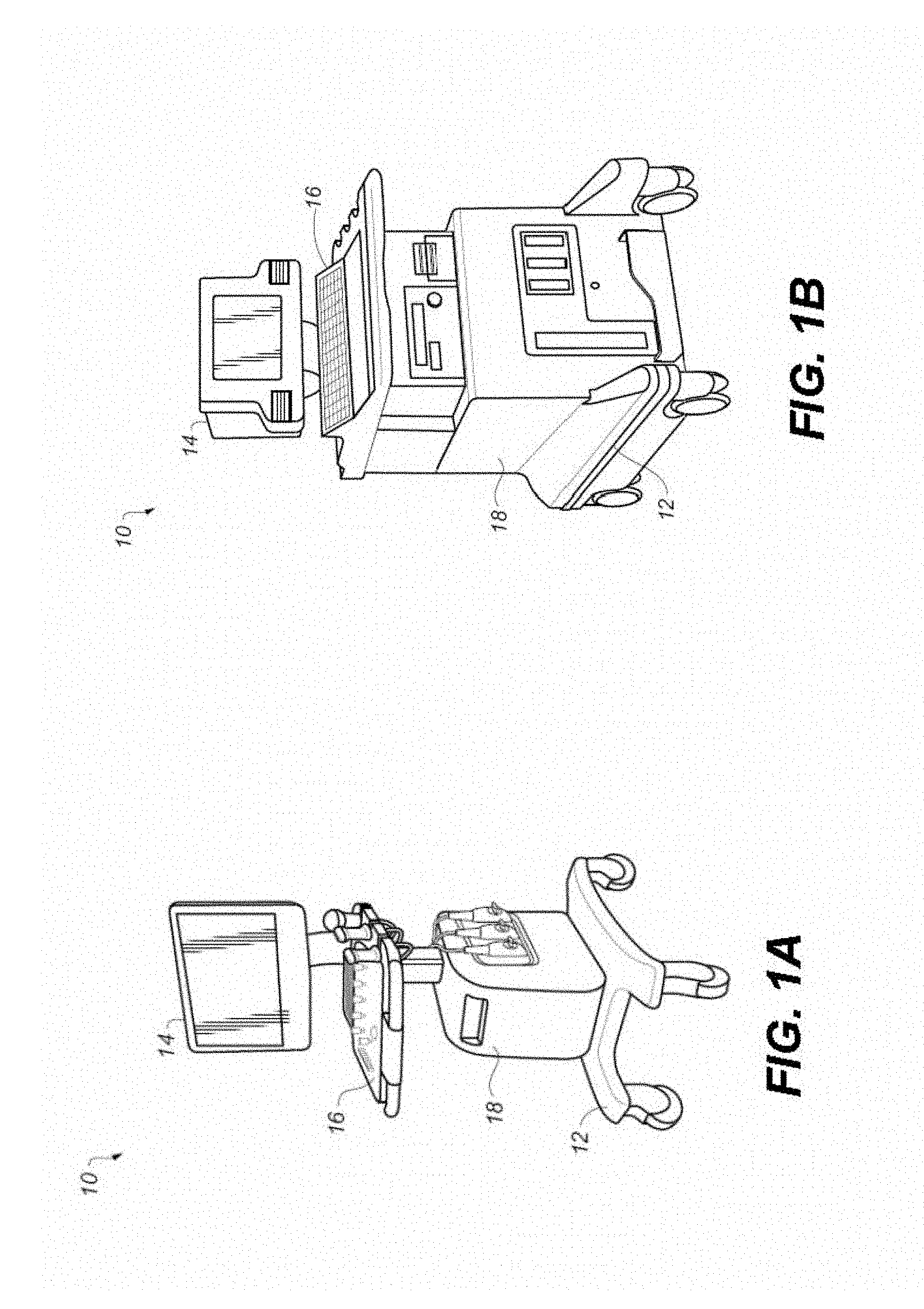
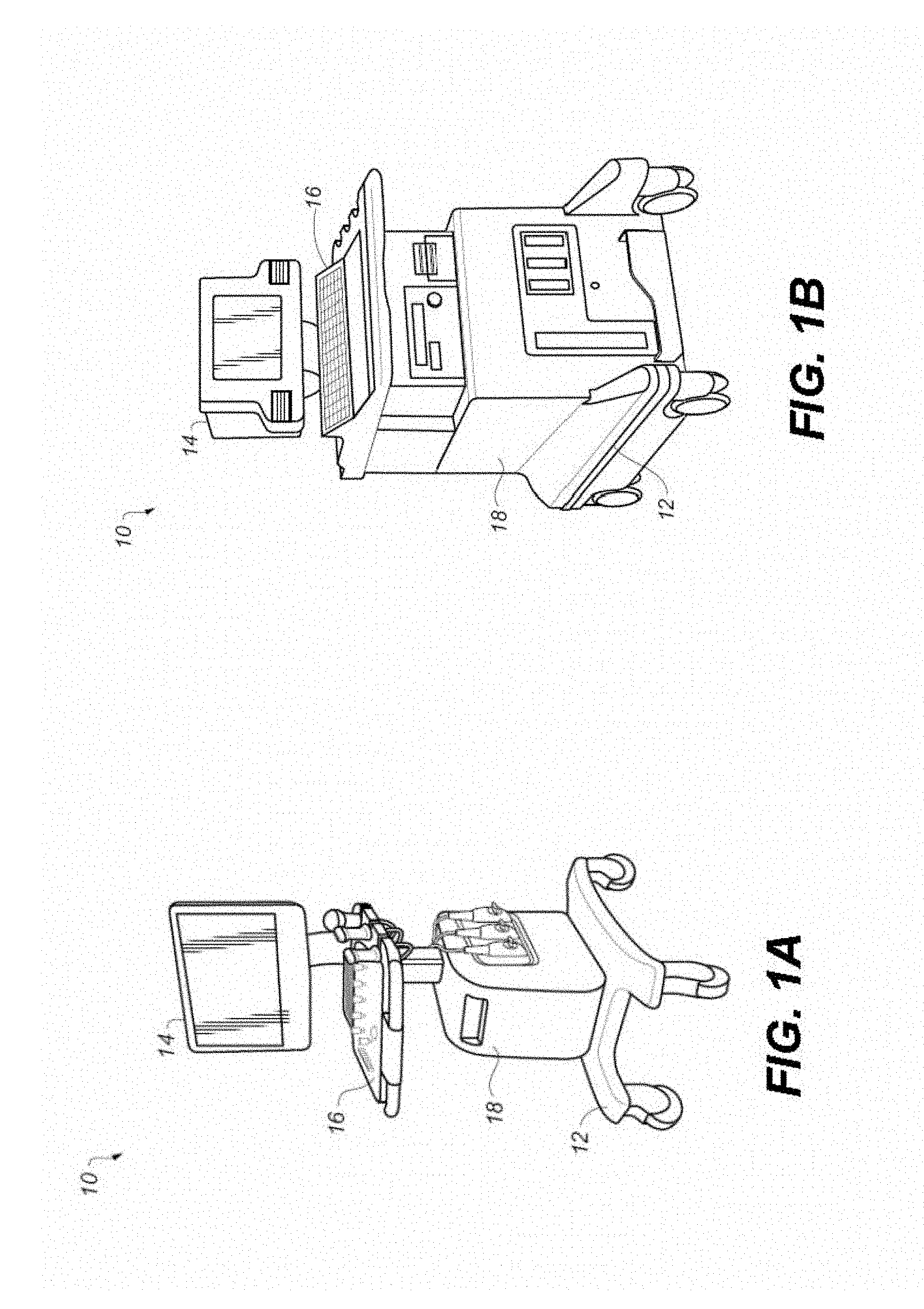
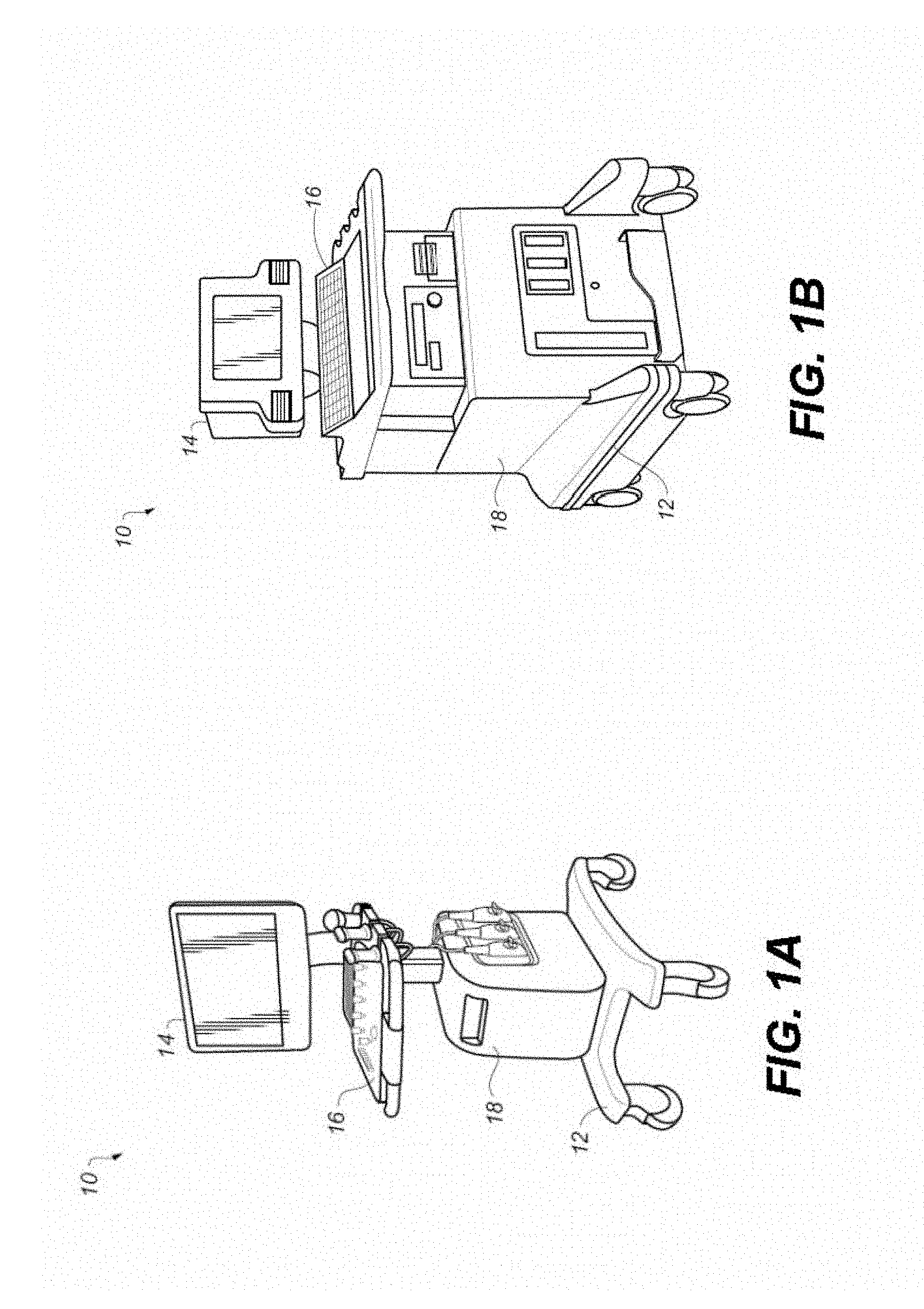
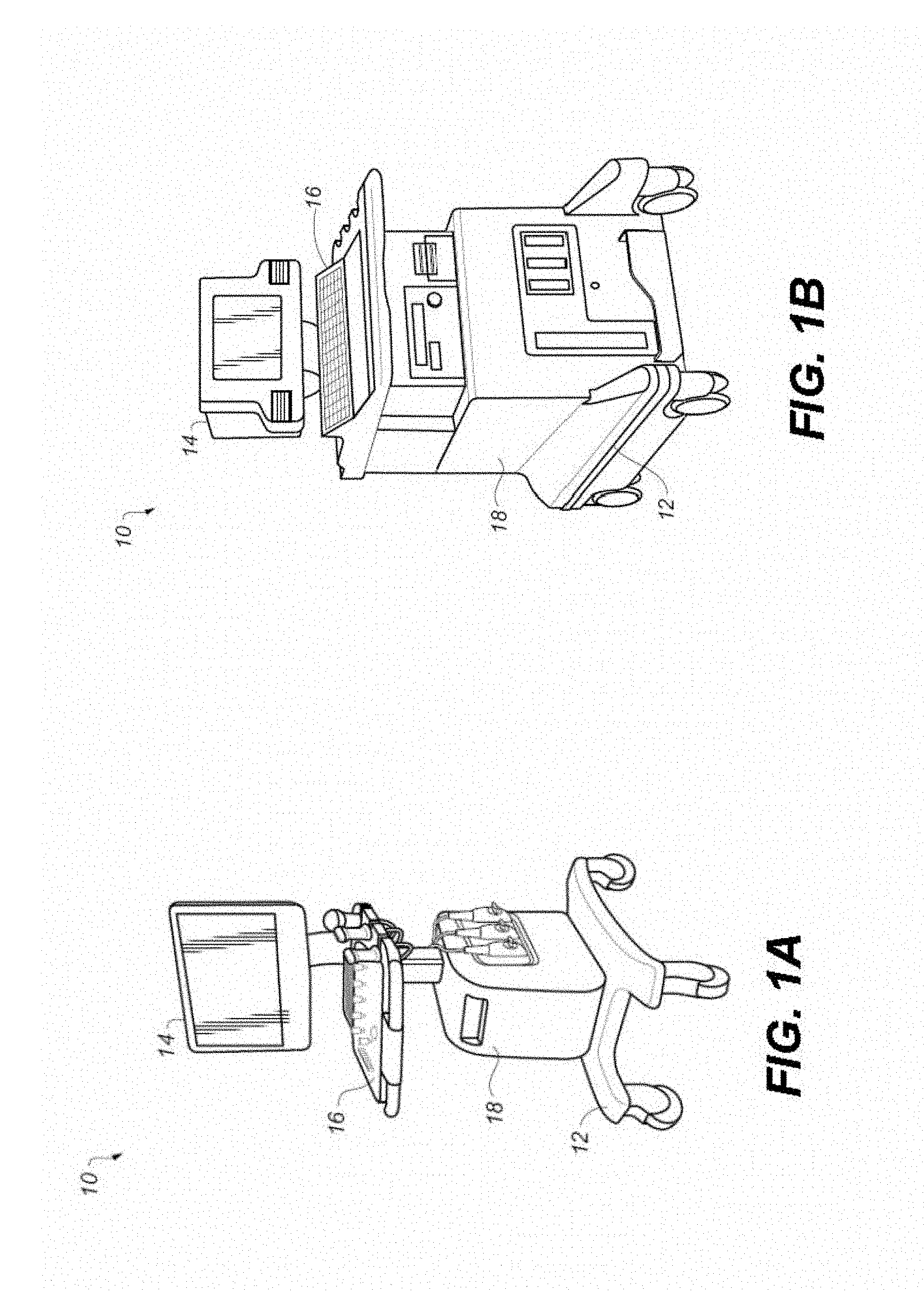
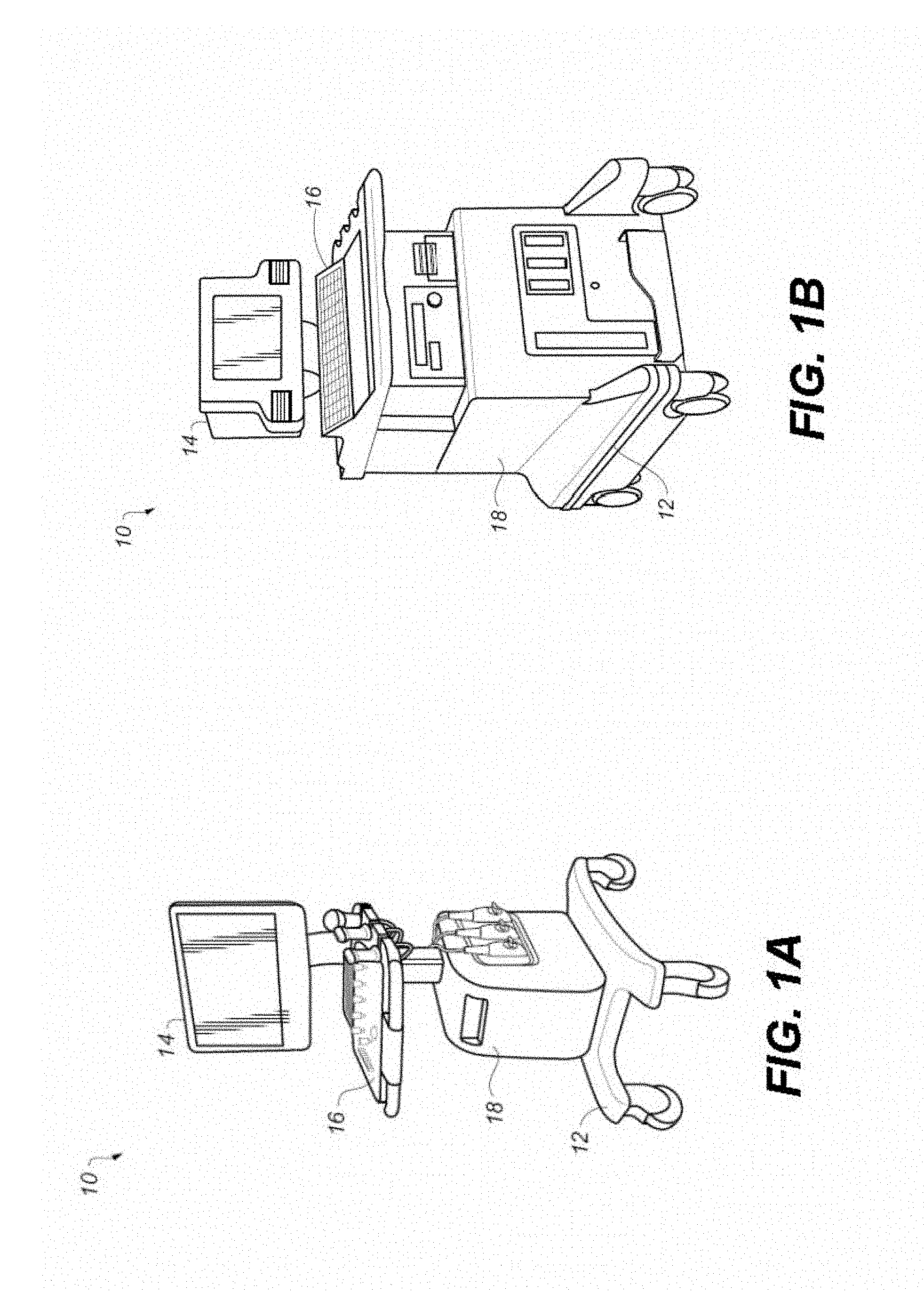
This application claims the benefit of U.S. Provisional application U.S. Ser. No. 62/598,494 provisionally filed on Dec. 14, 2017, entitled “ULTRASOUND SYSTEM AND METHOD FOR ACQUISITION PARAMETER DETERMINATION”, in the names of Ajay Anand and Michael Richards, incorporated herein by reference in its entirety. This application claims the benefit of U.S. Provisional application U.S. Ser. No. 62/525,777 provisionally filed on Jun. 28, 2017, entitled “ULTRASOUND SYSTEM AND METHOD FOR ACQUISITION PARAMETER DETERMINATION”, in the names of Ajay Anand and Michael Richards, incorporated herein by reference in its entirety. This research was funded in part by CEIS (Center for Emerging & Innovative Sciences), an Empire State Development-designated Center for Advanced Technology. The disclosure relates generally to the field of ultrasound systems and methods and more particularly to apparatus and methods that determine optimal acquisition parameters. More specifically, the disclosure relates to determining optimal acquisition parameters for ultrasound pulse wave imaging. Ultrasound imaging systems/methods are known medical devices, such as those described, for example, in U.S. Pat. No. 6,705,995 (Poland), U.S. Pat. No. 5,370,120 (Oppelt), US 2015/0141821 (Yoshikawa), and U.S. Pat. No. 8,285,357 (Gardner), all of which are incorporated herein in their entirety. Various applications for diagnostic ultrasound systems are given, for example, in the article entitled “Ultrasound Transducer Selection In Clinical Imaging Practice”, by Szabo and Lewin, Ultrasound utilizes sound waves at frequencies higher than those perceptible to the human ear. Ultrasonic images known as sonograms are generated as a result of pulsed ultrasonic energy that has been directed into tissue using a probe. The probe obtains echoed sound energy from the internal tissue and provides signal content that represents the different sound reflectivity exhibited by different tissue types. This signal content is then used to form images that visualize features of the internal tissue. Medical ultrasound, also known as diagnostic sonography or ultrasonography, is used as a diagnostic imaging technique used to help visualize features and operation of tendons, muscles, joints, vessels and internal organs of a patient. A number of advanced diagnostic tools have been demonstrated, based on continuing developments in ultrasound emission and detection, along with ongoing improvements in computation speed and in image processing and presentation techniques. Of particular interest for cardiovascular applications, for example, is the development and use of ultrasound signals for noninvasive characterization of arterial stiffness within local anatomical regions. This topic has been widely discussed in the modern biomedical ultrasound literature. Background information of particular interest can be found in the following references: (1) Jordi Calabia et. al. “Doppler ultrasound in the measurement of pulse wave velocity: agreement with the Complior method” published in It has been found that large arteries are not simple tube conduction structures. These arteries help to moderate systolic pressure increases and maintain sufficient diastolic level to guarantee myocardial perfusion. With the identification of new diseases and risk factors, it has been seen that these arteries lose their natural elasticity leading to high systolic and low diastolic blood pressure levels, which determine high pulse pressure. Arterial stiffness is being recognized as a useful biomarker for evaluating cardiovascular risk and for detection of incipient vascular disease. Recent research suggests that this parameter can serve as an independent predictor of cardiovascular mortality among elderly, hypertensive, and diabetic patients, among patients having chronic renal failure, and in the general population. Guidelines of the European Societies of Hypertension and Cardiology (2007-2009) postulate arterial stiffness assessment, measurement of the carotid plaque and ankle/brachial index as markers of vascular status. Any change in measured values may define a state of vasculopathy that significantly increases patient risk. Among methods for evaluating arterial stiffness, the most widely used metric in the literature is aortic pulse wave velocity (PWV). PWV relates to the speed at which the pulse wave travels on an arterial segment. PWV is often measured over the region that extends from the aortic arch or common carotid artery to the common femoral artery. PWV can be measured in a number of ways. In some methods, PWV is estimated as the ratio between change in flow (Q) and change in cross-sectional area (A) (PWV=dQ/dA) during the reflection-free period of the cardiac cycle. Conventionally, the pulse wave velocity measurement itself has been obtained using pressure transducers or employing arterial tonometry. Ultrasound signals have been used for PWV evaluation using carotid-femoral PWV measurements. Pulsed Doppler ultrasound measurements, using a linear array probe, are timed with ECG (electrocardiogram) or other biometric signals at the carotid artery and at the femoral artery. The pulse wave transit time is computed and averaged to obtain measured data. Pulse Wave Imaging (PWI) using ultrasound is well suited for localized measurements and is generally more sensitive to changes in local pathology than are more global measurement modes. For PWI, ultrasound signals are acquired at high frame rates, with arterial wall displacement computed using cross-correlation methods. PWV imaging, however, can be particularly sensitive to various acquisition parameters used by the operator, including frame rate. The optimal frame sampling rate for one patient or for one anatomical region may not be well suited for use with a different patient or over a different anatomical region, even for the same patient. This is because the optimal settings depend on the propagation velocity of the pulse wave that, in turn, depends on the local vessel wall properties, disease state of the blood vessel, and the overall hemodynamic status of the patient. The sonographer or other operator may have little experience or guidance in selecting the appropriate frame rate or related operational parameter for a PWV exam. Thus, it can be appreciated that methods for sensing and determining the appropriate frame rate and other suitable parameter data can be of particular value for effective delivery and measurement of PWV signals. An object of the present disclosure is to advance the art of ultrasound imaging and overall ultrasound system operation, directed more particularly to pulsed wave imaging. These objects are given only by way of illustrative example, and such objects may be exemplary of one or more embodiments of the invention. Other desirable objectives and advantages inherently achieved may be apparent to those skilled in the art. The invention is defined by the appended claims. According to one aspect of the disclosure, there is provided a method for ultrasound imaging comprising: a) acquiring an initial set of ultrasound images of a region of interest at an initial time t0 using a pulsed wave velocity imaging mode; b) acquiring one or more subsequent sets of ultrasound images in pulsed wave velocity imaging mode over the same region at a predetermined frame rate; c) computing a relative vessel wall displacement induced by pulse waves between frames acquired in a) and b); d) generating a pulse wave velocity distribution according to the computed displacement by comparing arrival times of the pulse wave at two different locations within the region of interest; e) identifying a subset of pulse wave velocity values from the distribution according to standard deviation or other statistical criterion; f) computing statistical results according to the subset of pulse wave velocity values; and g) displaying the computed statistical results on a display. The foregoing and other objects, features, and advantages of the invention will be apparent from the following more particular description of the embodiments of the invention, as illustrated in the accompanying drawings. The elements of the drawings are not necessarily to scale relative to each other. The following is a detailed description of the preferred embodiments, reference being made to the drawings in which the same reference numerals identify the same elements of structure in each of the several figures. Where they are used in the present disclosure, the terms “first”, “second”, “third”, and so on, do not necessarily denote any ordinal or priority relation, but are simply used to more clearly distinguish one element from another. Medical ultrasound (also known as diagnostic sonography or ultrasonography) is a diagnostic imaging technique based on the application of ultrasound, used to display internal body structures such as tendons, muscles, joints, vessels and internal organs. The ultrasound system, shown by way of example in Different types of images can be formed using sonographic instruments. The most well-known type is a B-mode image, which displays the acoustic impedance of a two-dimensional cross-section of tissue. Other types of image can display blood flow, motion of tissue over time, the location of blood, the presence of specific materials, the stiffness of tissue, or the anatomy of a three-dimensional region. Accordingly, the system of Clinical modes of ultrasound used in medical imaging include the following:
A sonographer, ultrasonographer, clinician, practitioner, or other clinical user, is a healthcare professional (often a radiographer but may be any healthcare professional with the appropriate training) who specializes in the use of ultrasonic imaging devices to produce diagnostic images, scans, videos, or 3D volumes of anatomy and diagnostic data. As noted in the background material given earlier, measurement of the aortic pulse wave velocity (PWV) is regarded as very useful in the region extending from the aortic arch or common carotid artery to the common femoral artery. As shown schematically in The transit time measures the time of travel of the foot of the wave over a known distance. Transit time Δt is estimated by the foot-to-foot method. The foot of the wave is defined at the end of diastole, where the steep rise of the waveform begins. Measurement methods have been shown to be highly reliable, but present disadvantages. Measurement requires specific devices and software and may not always be accurate in practice, due to difficulties in reliably recording pulse wave signals. Furthermore, the time required for the exploration is not negligible. In practice, one of the limitations of conventional test methods is that a global PWV estimate is provided. As invasive testing has shown, PWV varies significantly along the entire arterial tree due to variations in both the geometry and structure of the arteries. Therefore, the carotid-to-femoral PWV estimate represents an average of the local PWV values all along this arterial segment. Different arteries tend to stiffen at different rates and magnitudes during aging, with central arteries undergoing significantly higher stiffening than peripheral arteries. More importantly, a large number of pathologies result in localized arterial stiffening. For these reasons, it can be of particular value to measure PWV locally. A number of imaging methods have been proposed for the purpose of estimating PWV locally, primarily using MRI (magnetic-resonance imaging) and ultrasound. Pulse Wave Imaging (PWI) using ultrasound has been previously reported in the literature for both qualitative visualization of the pulse wave propagation in real time and for quantitative estimation of the PWV within the imaged arterial segment. PWI relies on tracking the arterial wall displacement using cross-correlation methods on RF ultrasound signals acquired at high frame rates. Measurements of Pulse Wave Velocity (PWV) have been found particularly useful for this purpose, allowing more precise information on circulatory condition over various regions of the anatomy to be obtained. Noninvasive quantification of regional arterial stiffness, such as can be derived from measurement of the Pulse Wave Velocity (PWV), has been considered to be of considerable clinical value. Pulse waves are flow velocity, pressure, and diameter waves generated at the ejection phase of the left ventricle. In an idealized model, the propagation speed of the wave (i.e., the PWV) is directly related to the Young's modulus of the artery or other blood vessel. Young's modulus, also known as the elastic modulus, provides a measure of material stiffness. Ultrasound-based techniques have been developed to measure the Pulse Wave Velocity for its diagnostic value. The ultrasound-based measurement provides a local or regional estimate that is viewed by some practitioners to be more readily correlated with spatial positions on an artery compared to global estimates conventionally obtained with non-imaging techniques. The ultrasound-based approach can be further extended to image the pulse wave such that the propagation patterns of the pulse wave can be visualized in addition to obtaining a single PWV value. Pulse Wave Imaging (PWI) has been investigated as a tool for characterizing the propagation of the pulse wave along the aorta and estimating the regional PWV. Related clinical applications include detection of abdominal aortic aneurysms and subsequent follow up. The ultrasound approach is based on tracking micron-sized displacements that are induced by the propagating pulse wave as it moves along the vessel wall. The displacement estimation approach is sometimes referred to as speckle tracking, and can be implemented by tracking the echo shifts in the radio frequency signal. A variety of methods have been proposed in the literature that are based on classic time-delay estimation, and phase tracking using autocorrelation-based estimators. The displacement estimation is performed at each of several lateral locations along the vessel wall over the extent of the lateral transducer width. Depending on the exact algorithm that is used, several adjacent lateral locations could be included in estimating a single PWV estimate. At each lateral vessel wall location, the temporal displacement profile has a sharp rise to peak displacement, followed by a transient decay back to baseline. One approach is to record the time instant when the sharp displacement rise (“knee of the waveform”) occurs and thus create a regression plot of arrival time as a function of lateral distance. The slope of the curve then provides an indicator of pulse wave velocity. The greater the number of scanlines (i.e. lateral locations used in the slope estimation), the lower the expected variance in the calculated velocity estimate. Although algorithms that perform the displacement estimation are straightforward, the accuracy of the resulting estimates depends on a variety of acquisition parameters. One parameter is the acquisition frame rate. Since the pulse wave displacement waveform has sharp transient characteristics (i.e. rapid rise and fall times) and since the entire pulse wave traverses a single location within tens or few hundreds of milliseconds, the waveforms need to be sufficiently well-sampled in order to be able to detect the features of interest (such as the “knee” of the waveform, described previously). Conversely, if the frame rate is very high, the inter-frame displacement is small. This, in turn, affects the accuracy of the displacement estimates because of challenges in tracking very small displacements that can be close to the noise floor. Judicious choice of the inter-frame time interval is thus desired, considered important for promoting reliable tracking of the displacements without introducing jitter, bias, and other undesirable tracking errors. Moreover, in a diseased artery, since the pulse wave velocity increases due to stiffening and the waveform shape changes as well, it may not be possible to characterize a priori the optimal frame rate for use in particular clinical situations. Applicants have recognized, from recent ex vivo data acquired by Applicants during the course of research, the variability of the pulse wave velocity estimates with frame rate (Frames Per Second, or FPS), as illustrated in Table 1 below. Applicants' data was acquired in a flow phantom setup with an aorta model fabricated using 10% PVA polymer (Polyvinyl alcohol). In a clinical setting, this relative level of variability in measurement can be highly troubling, raising concerns about data validity and causing some confusion about which value may be correct. Applicants' method addresses this problem by proposing a workflow approach that improves confidence in determining the correct PWV value or range, and guides the user to the optimal set of acquisition parameters. For example, in one configuration, the Applicants' method is integrated into software developed to implement Pulse Wave Imaging on a medical ultrasound system. Applicants' method determines the optimal frame rate or range of frame rates which provides the preferred/desired/accurate value for the Pulse Wave Velocity in the clinical situation being imaged. Applicants' method can be implemented using one or more of the steps described following and shown in summary in the logic flow diagram of In an acquisition step S400, acquire ultrasound echo data at the highest allowable frame rate. Set an initial time (for example, t0) to represent an instant prior to the onset of the pulse wave at a particular location. In a computation step S410, compute the displacement (or velocity) at each spatial lateral location using two or more different displacement calculation schemes, for example: (a) Frame-to-frame, in a sampling pattern that does not skip frames from adjacent acquisitions. This allows computation of the incremental relative displacement between adjacent frames and accumulates a running total that is indicative of the total displacement at every frame time. (b) Frame-to-frame, with frame skipping. The frame-to-frame displacement is computed but with sampling at different time intervals, skipping frames in a sequence that effectively increases the magnitude of the displacement computed in every pair of frames compared. As in scheme (a), total displacement is estimated by cumulatively adding displacements from each pair of frames compared; however, in scheme (b) the sampling pattern is different. Scheme (b) can be repeated by systematically skipping a different number of frames in each iteration, up to a predefined maximum. (c) Reference-frame based acquisition. Here, the total displacement is calculated by comparing each sampled frame with respect to frame 1 that is nominally acquired at initial time t0 and that represents the initial position. Computation step S410 can optionally be repeated for some portion or all of the lateral locations. In an initial distribution generation step S420, a PWV value is computed using each of the approaches applied in step S410 (step 2, above). A distribution of the candidate PWV values is then obtained as an initial set of PWV values. A discard step S430 can effectively discard outlier values from the distribution in order to generate a subset of pulse wave velocity values. In practice, it has been found that a subset of the PWV values cluster together with minimal variability, while outlier values resulting from sub-optimal frame comparison choices are nominally separated from the cluster. These outlier values can be removed from subsequent computation and analysis. Statistical measurements can be used to identify a subset of pulse wave velocity values usable for subsequent computation, such as values within a predetermined standard deviation (SD) of a mean value, for example. In an optional filtering step S440, other metrics such as using cross-correlation coefficients (computed during the displacement estimation for each of the approaches in Step 2) can be used as a filter to further reduce the subset of candidate values from the clustered subset obtained in Step 4 above. In a reporting step S450, following outlier removal from earlier processing, a range from the cluster of PWV values, such as a mean value +/−standard deviation, or other descriptive statistic that is representative of the cluster (including median, mean, and other statistics) can be reported, displayed to the operator or stored for future processing. Various frame selection schemes for frame sampling, described above with relation to the According to an embodiment, the calculated pulse wave velocity distribution can be used to automate selection of a suitable frame rate for subsequent PWV imaging for a particular location. Applicants' method can be configured/arranged as a computer medium or software package integrated with the main system software for pulse wave imaging on a medical ultrasound system. The approach can also be applied to other ultrasound imaging modes (such as strain elastography, vessel wall distension measurements, and the like) where displacements are estimated from ultrasound echo data and optimal range of frame rates for data sampling is significant. A computer program product may include one or more storage medium, for example; magnetic storage media such as magnetic disk (such as a floppy disk) or magnetic tape; optical storage media such as optical disk, optical tape, or machine readable bar code; solid-state electronic storage devices such as random access memory (RAM), or read-only memory (ROM); or any other physical device or media employed to store a computer program having instructions for controlling one or more computers to practice the method according to the present invention. The invention has been described in detail, and may have been described with particular reference to a suitable or presently preferred embodiment, but it will be understood that variations and modifications can be effected within the spirit and scope of the invention. The presently disclosed embodiments are therefore considered in all respects to be illustrative and not restrictive. The scope of the invention is indicated by the appended claims, and all changes that come within the meaning and range of equivalents thereof are intended to be embraced therein. A method for ultrasound imaging acquires an initial set of ultrasound images of a region of interest at an initial time t0 using a pulsed wave velocity imaging mode and one or more subsequent sets of ultrasound images in pulsed wave velocity imaging mode over the same region at a predetermined frame rate. The relative displacement between acquired frames is computed. A pulse wave velocity distribution is generated according to the computed displacement by comparing arrival times of the pulse wave at different locations over the region. A subset of pulse wave velocity values from the distribution is identified according to standard deviation or other statistical criterion. Statistical results are computed according to the subset of pulse wave velocity values. Computed statistical results are displayed. 1. A method for ultrasound imaging, comprising:
a) accessing an initial set of ultrasound images of a region of interest at an initial time t0 acquired using a pulsed wave velocity imaging mode; b) accessing at least one subsequent set of ultrasound images of the region of interest acquired using a pulsed wave velocity imaging mode at a predetermined frame rate; c) computing a relative vessel wall displacement induced by pulse waves between frames acquired in steps a) and b); d) generating a pulse wave velocity distribution according to the computed relative vessel wall displacement by comparing arrival times of the pulse wave at two different locations within the region of interest; e) identifying a subset of pulse wave velocity values of the generated pulse wave velocity distribution according to a statistical criterion; f) computing at least one statistical result according to the identified subset of pulse wave velocity values; and g) displaying, on a display, the computed at least one statistical result. 2. The method of 3. The method of 4. A computer storage medium having instructions stored therein for causing a computer to perform the method of 5. A computer product embodied in a computer readable medium for performing the steps of 6. A computer storage product having at least one computer storage medium having instructions stored therein causing one or more computers to perform the method of 7. A method, comprising:
acquiring, at a predetermined acquisition frame rate, a first set and a second set of ultrasound echo data, each acquired set of ultrasound echo data acquired at a corresponding spatial lateral location of a blood vessel unique to the set; generating a distribution of pulse wave velocity estimates according to the first and a second sets of the ultrasound echo data; identifying a set of pulse wave velocity values from the generated pulse wave velocity distribution according to a statistical criterion; computing at least one statistical result according to the identified set of pulse wave velocity values; and reporting the at least one statistical result. 8. The method of computing the pulse width velocity of the acquired frames; and comparing arrival times of the pulse wave at the corresponding first spatial lateral location to arrival times at the second spatial lateral location along the blood vessel. 9. The method of 10. The method of 11. The method of 12. The method of 13. The method of 14. The method of CROSS REFERENCE TO RELATED APPLICATIONS
SPONSORED RESEARCH AND DEVELOPMENT
TECHNICAL FIELD
BACKGROUND
SUMMARY
BRIEF DESCRIPTION OF THE DRAWINGS
DETAILED DESCRIPTION OF THE EMBODIMENTS
557 4.53 145.9 1055 2.79 55.2 1908 2.72 52.6 Sequence for Frame Rate Determination