MULTIFUNCTIONAL BIODEGRADABLE PEG NANOCARRIER-BASED HYDROGELS FOR PREVENTING HIV TRANSMISSION
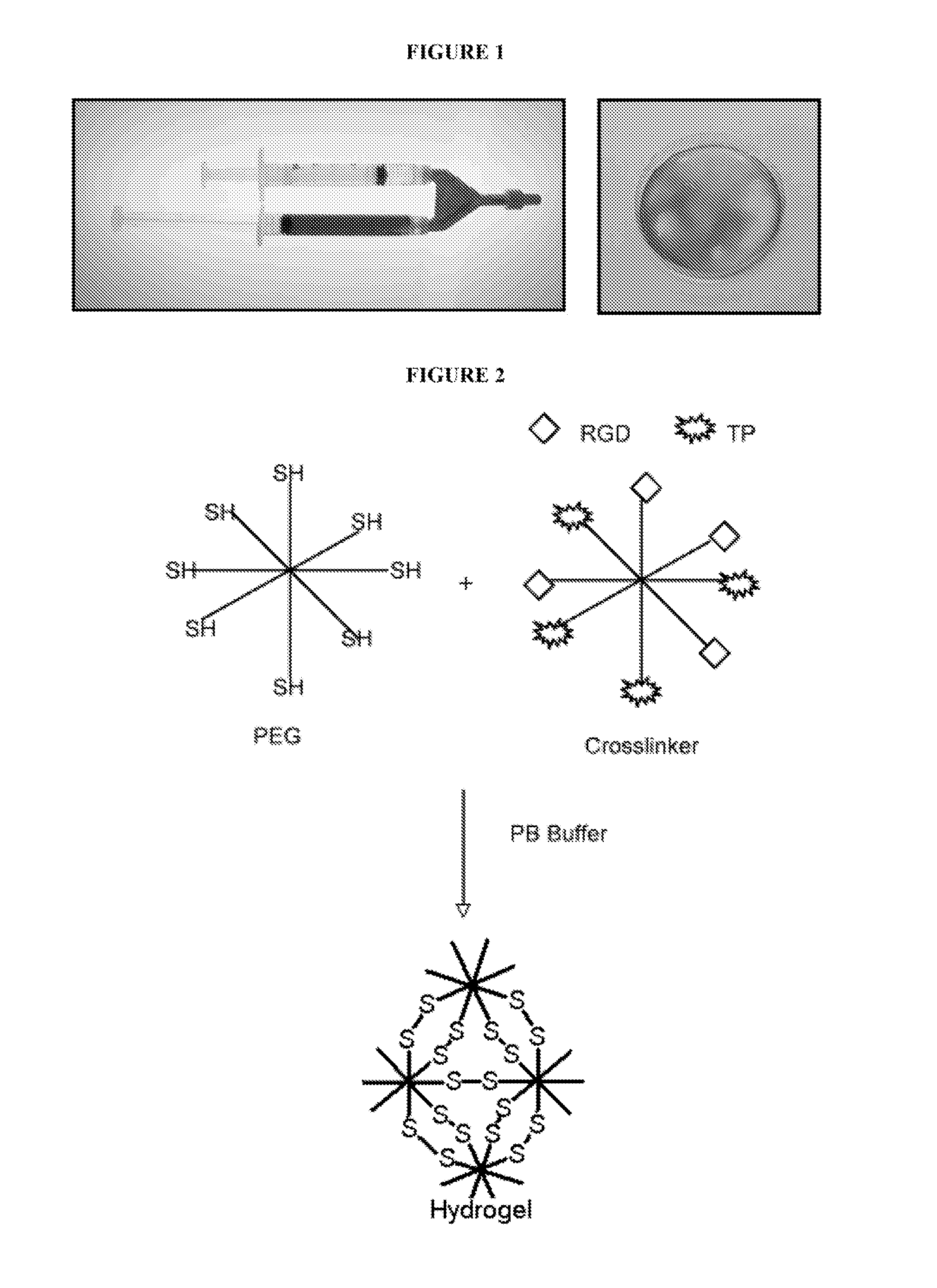
This application claims priority under 35 U.S.C. §119(e) to U.S. Provisional Application Ser. No. 61/413,652, which was filed on Nov. 15, 2010 and U.S. Provisional Application Ser. No. 61/436,320, which was filed on Jan. 26, 2012. The disclosures of both applications are incorporated herein by reference. This invention was made with government support under R01AI084137-01 awarded by the National Institutes of Health HIT-IT program. This invention was also made with government support under NCCAM NIH R21AT002897-01 awarded by the National Institutes of Health. The government has certain rights in the invention. Bacterial vaginosis (BV) is a common condition characterized by an imbalance in the vaginal microflora, where healthy lactobacilli are replaced by a proliferation of facultative and anaerobic microorganisms, most notably It has been estimated that between 10-30% of women in North America are afflicted by this ailment, frequently prompting them to seek medical attention. Although BV often remains asymptomatic, the unrestricted growth of these organisms has been demonstrated to have pathogenic effects, particularly in pregnant women. BV is associated with the development of pelvic inflammatory disease, as well as a variety of pregnancy-related complications, including low fetal birth weight, preterm births with an elevated risk of infant death, intra-amniotic infections leading to fetal brain damage, and spontaneous abortion. Additionally, Bacterial vaginosis, and With the incidence of HIV infection on the rise, the development of vaccines and topical microbicides has been a major worldwide priority. However, the results of recent trials have been disappointing. As such, the induction of sterilizing immunity and protection against HIV infection continues to be a major public health goal. “Microbicides,” topically applied agents that prevent HIV transmission from person to person, are still believed to hold considerable promise. In fact, it has been estimated that a microbicide used 50% of the time by 20% of women at risk could prevent 2.5 million HIV infections in 3 years. Given recent clinical developments, there is an urgent need to rethink the concept of microbicides. The present invention is directed to a multifunctional polyethylene glycol-based hydrogel that includes a multi-arm polyethylene glycol cross-linking unit covalently bound to at least four multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit includes an agent coupled to the nanocarrier unit and each agent is selected from pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding, provided that each nanocarrier unit comprises a different agent. at least two nanocarrier units comprise an agent having a different functionality. In one embodiment, at least one agent is coupled to a nanocarrier unit via a degradable bond. In another embodiment, at least one agent is coupled to a nanocarrier via a nondegradable bond. In yet another embodiment, the hydrogel includes a pH-lowering agent selected from lactic acid, citric acid, ascorbic acid, and maleic acid. In one embodiment, the hydrogel includes a pH-lowering agent encapsulated in a carrier. In another embodiment, the carrier is cyclodextrin, a dendron, a dendrimer, a liposome, or a PEG nanogel particle. In yet another embodiment, the hydrogel includes subtilosin. In yet another embodiment, the hydrogel includes an agent that inhibits free and cell-associated HIV binding selected from soluble polyanions and an RGD peptide ligand. In another embodiment, the soluble polyanion is selected from dextran sulfate, cyclodextrin sulfate, and heparin. In yet another embodiment, the hydrogel includes at least one nanocarrier unit noncovalently bound within the hydrogel. The present invention also relates to a method for preparing a hydrogel by combining an amount of multi-arm polyethylene glycol cross-linking units that include a thiol-reactive functional group coupled to each arm with an amount of multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit includes a thiol group coupled to half of the arms and an agent coupled to the remaining arms of each nanocarrier unit and each agent is selected from pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding; wherein said amounts of the cross-linking units and the nanocarrier units are sufficient to produce a hydrogel when combined. In one embodiment, each nanocarrier unit that is combined with the same polymer unit includes a different agent. Also presented is a kit for use in preparing a multifunctional polyalkylene oxide-based hydrogel that includes: (a) an amount of multi-arm polyethylene glycol Cross-linking units that include a thiol-reactive functional group coupled to each arm; and (b) an amount of multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit includes a thiol group coupled to half of the arms and an agent coupled to the remaining arms of each nanocarrier unit and each agent is selected from pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding; wherein the amounts of the cross-linking units and the nanocarrier units are sufficient to produce a hydrogel when combined. Also provided is a method for prophylactically reducing the risk of development of HIV in a patient by intravaginally or intrarectally administering to a patient: (a) an amount of multi-arm polyethylene glycol cross-linking units that include a thiol-reactive functional group coupled to each arm; and (b) an amount of multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit includes a thiol group coupled to half of the arms and an agent coupled to the remaining arms of each nanocarrier unit and each agent is selected from pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding; wherein the amounts of the cross-linking units and the nanocarrier units are sufficient to produce a hydrogel when combined. Also provided is an article that includes the hydrogel of the present invention. Another embodiment includes a topical composition that includes an anti-microbial and/or spermicidal effective amount of subtilosin incorporated into a pharmaceutically acceptable aqueous solution, non-aqueous solution, nanofiber, hydrogel, gel, nanogel, suspension, ointment, jelly, insert, suppository, sponge, salve, cream, foam, foaming tablet, or douche. The present invention relates to a multiplex nanocarrier-based polyethylene glycol (PEG) vaginal hydrogel for preventing the initial infection (i.e., acquisition) and dissemination of HIV through the vaginal mucosa to distant tissues. The multiplex hydrogel matrix is formed by crosslinking various PEG nanocarriers, each of which plays a different role in the functional properties of the hydrogel (e.g., promoting mucosal adhesion, maintaining mildly acidic pH, releasing microbicide and spermicides, and preventing HIV virion binding). Hydrogels are formed by intermolecular cross-linking of hydrophilic polymers. They are capable of absorbing large amounts of water and swelling, while maintaining their three-dimensional networks. Molecules of different sizes can diffuse through the hydrogel matrix, which resembles living tissue due to the hydrogel's high-water content and soft/rubbery characteristics. Hydrogels are used in drug delivery, tissue engineering, and imaging applications. The current polymer and crosslinker nanocarriers are based on polyethylene glycol, which is a water soluble, nontoxic and biocompatible polymer. This is particularly important since disruption of the mucosa (tissues and normal vaginal flora has been associated with increased rates of HIV-1 acquisition and shedding. The hydrogel is a liquid upon instillation allowing for high vaginal dispersion and mucosal coverage where it then undergoes a rapid phase transition to form a visco-elastic hydrogel that does not depend upon temperature or pH. The multiplex hydrogel matrix is formed by crosslinking various PEG nanocarriers each of which plays a different role in the functional properties of the hydrogel (e.g., promoting mucosal adhesion, maintaining mildly acidic pH, releasing microbicides and spermicides, and preventing HIV virion binding). It has been shown that (1) sexually transmitted and vaginal infections such as bacterial vaginosis (BV) increase the risk of HIV transmission by weakening mucosal barriers and by stimulating an inflammatory response that may activate or recruit HIV target cells to the portals of viral entry, (2) low vaginal pH (<4.5) inactivates HIV and inhibits CD4+ lymphocyte activation, thus reducing the number of HIV target cells in the vagina, and (3) cell-associated HIV breaches the normal stratified squamous epithelial barrier of the vagina with low frequency. Preferably, the hydrogel of the present invention imparts a robust physical barrier, restores the natural microbicidal vaginal barrier functionality, and prevents HIV binding. It is also preferred that the hydrogel is colorless, odorless, inexpensive to manufacture, safe to use more than once a day and for long periods of time, fast-acting, undetectable to either partner, and available in contraceptive and noncontraceptive forms. For example, the hydrogel can be applied directly to the vagina or rectum. The hydrogel of the invention may also be impregnated into absorptive substrate materials, such as sponges, or coated onto the surface of solid substrate materials, such as male or female condoms, diaphragms, cervical caps, or medical gloves, to deliver the compositions to vaginal or other potentially infectable epithelium. Other articles and delivery systems of this type will be readily apparent to those skilled in the art. As used herein, “condom” refers to a barrier device which is used to provide a watertight physical barrier between male and female genitalia during sexual intercourse, and which is removed after intercourse. This term includes conventional condoms, which cover the penis; it also includes so-called “female condoms” which are inserted into the vaginal cavity prior to intercourse. Preferably, condoms should be made of latex or a synthetic plastic material such as polyurethane, since these provide a high degree of protection against viruses. Also provided is a method for prophylactically reducing the risk of development of HIV in a patient by intravaginally or intrarectally administering to a patient: (a) an amount of multi-arm polyethylene glycol cross-linking units that include a thiol-reactive functional group coupled to each arm; and (b) an amount of multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit includes a thiol group coupled to half of the arms and an agent coupled to the remaining arms of each nanocarrier unit and each agent is selected from pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding; wherein the amounts of the cross-linking units and the nanocarrier units are sufficient to produce a hydrogel when combined. In one embodiment of the present invention, an 8-arm PEG polymeric nanocarrier is crosslinked to form the hydrogel network entrapping water as the hydrogel forms. As a result, hydrogels resemble living tissue due to their high-water content and soft/rubbery characteristics. The PEG hydrogel can serve as a lubricant during sex. The basic PEG unit is identical for the “cross-linking” and “nanocarrier” units with two exceptions: (1) functional groups on the cross-linking unit (e.g. thiol-reactive functional groups, including but not limited to activated ester, activated thiol, maleimide, vinyl sulfone, and the like) and on the nanocarrier unit (e.g. thiol (—SH)) are complimentary so that they will react to form the hydrogel network and (2) in addition to the thiol-reactive functional groups, the nanocarrier units also possess various functionalities such as pH lowering units, bioadhesion units (e.g. xanthan gums, hydroxypropyl cellulose, carpools, polycarbophils, chitosan, alginates, and the like). microbicide & spermicide units or polyanionic and RGD units to block free and cell-associated HIV binding (e.g. antiviral). Mixing various nanocarrier units with the cross-linking unit forms the multiplex hydrogel, imparting the desired functional properties to the hydrogel. The nanocarrier units are prepared using multi-arm and/or branched PEG-thiol polymers. The number of thiol groups (e.g. arms) varies preferably from 2 to 16, more preferably from 2 to 8. The molecular weight of the thiol polymer ranges preferably from about 10,000 Da to about 100,000 Da, more preferably from about 10,000 Da to about 60,000 Da. The amount or nanocarrier units used to prepare the hydrogels of the present invention varies from about 2% w/v to about 40% w/v, more preferably from about 2% w/v to about 20% w/v. in one embodiment of the present invention, the hydrogel includes copolymers containing repeating units of thiol groups, e.g. poly[poly(ethylene glycol)-alt-poly(mercaptosuccinic acid)] having a molecular weight range from about 1,000 Da to about 100,000 Da. The cross-linking unit is either linear or a multi-arm (branched) polymer that includes thiol-reactive functional groups, such as, activated esters, activated thiols, maleimide, vinyl sulfone, and the like. The molecular weight range for the crosslinking unit preferably ranges from about 1,000 Da to about 40,000 Da, more preferably from about 2,000 Da to about 20,000 Da. The number of functional groups varies preferably from 2 to 8. The nanocarrier unit to cross-linking unit stoichiometry varies from 10:0.05 to 0.05:10. Currently marketed vaginal gels (e.g. Conceptrol II® and Gynol II®) are “soft” gels that use gelling agents such as sodium carboxymethylcellulose to increase their viscosity. As a result, soft gels have poor mechanical strength and are unable to maintain a robust physical barrier to pathogens. It is equally important that vaginal gels have good viscoelastic properties in order to resist structural changes under strain (e.g., during normal movement, sexual intercourse, etc.). If a gel cannot resist structural changes, openings will form in the gel allowing pathogens to invade the mucosa. To our knowledge, none of the gels that are currently marketed or are being developed have any significant elastic nature. It is also imperative that gels have high disperability and retention inside the vagina to insure maximal mucosal surface coverage. Physical gels have limited ability to spread and cover the mucosal surface once instilled into the vagina (i.e., spreading only occurs as the gel becomes diluted and less viscous making it an even less effective barrier). It is readily apparent that currently marketed vaginal gels were not designed to provide a good physical barrier to pathogens. The hydrogel of the present invention offers the advantage of being administered as a solution in order to get maximal vaginal mucosal coverage. However, unlike any of the commercially available gels, it then quickly forms a firm hydrogel of good viscosity, flexibility/elasticity and mechanical strength. The functional properties of the hydrogel of the present invention are customized by covalently linking an agent with a nanocarrier unit of the hydrogel or by passively (i.e., noncovalently) trapping it within the hydrogel matrix as it forms in situ. A higher loading capacity of an agent can be achieved by passive entrapment, however, high agent payloads may not always be needed. For example, if the goal is to maintain vaginal pH or slightly reduce pH then the covalently linked acids should be adequate because their release will be slow and sustained. If the goal is to dramatically reduce pH (e.g., during the initial treatment of BV) then higher “doses” with a shorter duration of release will be required. Passive entrapment can also be used to achieve this functionality. In one embodiment, one or more agents are functionalized with thiol-reactive functional groups, which include but are not limited to activated esters, activated thiols, vinyl sulfone, malemide, and the like to form either degradable thioester and disulfide bonds or stable (non-degradable) thioether bonds with the polymer. The number of agents attached to the polymer varies from preferably 1 to 8, more preferably from 1 to 4. In terms of amount, the agents account for thiol modification in the range of from about 10% to about 80%, more preferably from about 10% to about 60%. In one embodiment, noncleavable linkages are used for the HIV binding functionality whereas cleavable linkages are used for releasing therapeutic agents. Preferably, the hydrogel of the present invention restores a normal microbicidal vaginal environment and thus prevents HIV transmission by effectively maintaining acidic pH and treating BV infection. Vaginal infections such as BV and the introduction of semen, which is alkaline, into the vagina elevate pH above the critical pH (˜4.5) required to inactivate HIV and BV pathogens. The altered vaginal environment is favorable to HIV entry and transmission. Unfortunately, most attempts at maintaining acidic vaginal pH have failed due to poor delivery methods of the acidifying agent and/or low buffer capacity. The hydrogel of the present invention mimics the function of the natural vaginal environment by slowly releasing low amounts of lactic acid or other safe mild acids. Lactic acid is the preferred acidifying agent due to its natural function in the vagina. Lactic acid-nanocarriers are formed by reacting the N-hydroxysuccinimidyl ester of lactic acid with the —SH groups of the polymer via a thioester linkage. The thioester linkages degrade, slowly releasing lactic acid. At the pH of the diseased vagina (pH 5-7), lactic acid is preferably released over a period of 18-30 hours. Lactic acid is attached either directly or through a linker, which preferably 2-12, and more preferably 2-6 carbons long. The number of lactic acid moieties on the polymer varies preferably from 1 to 8, more preferably from 1 to 4. Citric, maleic, or ascorbic acid can also be used. The linker for citric acid is mercaptoethanol and 3-mercaptopropanoic acid for ascorbic acid. An alternative preparation is to encapsulate the acids in a carrier such as cyclodextrin, dendrons, dendrimers, liposomes, or PEG nanogel particles, such as those disclosed in International Publication No. WO2009123768, the contents of which are incorporated herein by reference, and passively entrap those particles in the hydrogel where they slowly release the acids. In another embodiment, the hydrogels of the present invention treat bacterial vaginosis (BV). In yet another embodiment, the hydrogels of the present invention prevent HIV binding to cells to reduce HIV transmission. Nonspecific attachment inhibitors can be active against both free- and cell-associated HIV. The first step of HIV binding involves the interaction with a target cell. This nonspecific adsorption/attachment process, which occurs before gp120 binding to CD4, is based on the interaction of the positively charged regions of Env with the negatively charged proteoglycans of the cell surface. Soluble polyanions, such as dextran sulfate, cyclodextrin sulfate, and heparin, have been shown to block the nonspecific attachment of HIV virions. A number of other polyanions have also been reported to have such activities as well. In another embodiment of the present invention, polyanionic nanocarriers are constructed by attaching negatively charged amino acids, which include but are not limited to Glu and Asp. These amino acids have two carboxylic groups (two negative charges). The amino acids are attached to the polymer either directly or through a linker, which is preferably 2-12, and more preferably 2-6 carbons long. The anionic amino acids are attached to the polymer preferably through non-degradable bonds. The number of amino acids on eight-arm thiol polymers varies from 1-8, more preferably from 1-4. Since each amino acid has two anionic charges, the negative charge on the nanocarrier ranges from 2-16, more preferably from 2-8. In another embodiment, charge density is increase 2-3 fold by using di- or tripeptide instead of amino acids. Other examples of polyanions include, but are not limited to, dextran sulphate, heparin sulfate, and the like. Another embodiment utilizes aggregated PEG nanogels ( Another binding interaction is based on the interaction of the peptide ligand RGD with αβ (e.g. αvβ3, α5β1, etc.) integrins on cell surfaces. It has been suggested that HIV-1 entry into the vaginal mucosal epithelial cells is more efficient when HIV-1 particles bud locally after contact between HIV-1-infected cells and uninfected mucosal epithelial cells rather than by direct entry of cell-free virus into the epithelial cells. This interaction, also true for CD4+ T-cells, is integrin and proeteoglycan agrin-dependent. In one embodiment of the present invention, the RGD-peptide is attached to the thiol polymer through non-degradable bonds. The RGD peptide is either linear or cyclic and is attached either directly or through linker, which is preferably 2-12, and more preferably 2-6 carbons long. The number of RGD peptide on the polymer varies, preferably from 1-8, and more preferably from 1-4. Preferably, the hydrogels in present invention also treat the HIV infection. The preferred therapeutic is nucleotide reverse transcriptase inhibitor (NRTI), tenofovir. Tenofovir is an analogue of adenosine monophosphate, and is characterized as acyclic nucleoside phosphate. Tenofovir is administered orally as prodrug, tenofovir disoproxil fumarate. It is converted to its active form, tenofovir diphosphate, intracellularly by phosphorylation, and acts as a chain terminator when HIV reverse transcriptase is actively making viral DNA. In one embodiment of the present invention, tenofovir is attached to the thiol polymer via degradable thioester bonds. Tenofovir is attached either directly or through linker, which is preferably 2-12, and more preferably 2-6 carbons long. The tenofovir moieties on the polymer vary preferably from 1-8, more preferably from 1-4. In another embodiment of present invention, a therapeutic agent is passively encapsulated into the hydrogel matrix. Other examples of therapeutic agents include, but not limited to, UC781; nucleoside reverse transcriptase inhibitors (NRTIs) like zidovudine, didanosine, zalcitabine, stavudine, lamivudine, abacavir sulfate, emtricitabine, etc.; non-nucleoside reverse transcriptase inhibitors (NNRTIs) like nevirapine, delaviridine, efavirenz, entavirine, etc.; protease inhibitors (PIs) like saquinavir mesylate, ritonavir, indinavir, nelfinavir mesylate, amprenavir, fosamprenavir calcium, atazanavir sulfate, lopinavir and ritonavir, tipranavir, darunavir, etc.; entry and fusion inhibitors like maraviroc, enfuviritide, etc.; and integrase inhibitors like raltegravir etc. Methods for preparing the hydrogels of the present invention are also presented. In one embodiment, the hydrogel is prepared by combining an amount of multi-arm polyethylene glycol cross-linking units that include a thiol-reactive functional group coupled to each arm with an amount of multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit includes a thiol group coupled to half of the arms and an agent coupled to the remaining arms of each nanocarrier unit and each agent is selected from pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding; wherein said amounts of the cross-linking units and the nanocarrier units are sufficient to produce a hydrogel when combined. In one embodiment, each nanocarrier unit that is combined with the same polymer unit includes a different agent. Also presented is a kit for use in preparing a multifunctional polyalkylene oxide-based hydrogel that includes: (a) an amount of multi-arm polyethylene glycol cross-linking units that include a thiol-reactive functional group coupled to each arm; and (b) an amount of multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit includes a thiol group coupled to half of the arms and an agent coupled to the remaining arms of each nanocarrier unit and each agent is selected from pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding; wherein the amounts of the cross-linking units and the nanocarrier units are sufficient to produce a hydrogel when combined. The present invention also relates to methods for prophylactically reducing the risk of development of bacterial vaginosis in a patient by intravaginally administering a composition to the patient that includes a bacterial vaginosis prophylactic effective amount of subtilosin. In another embodiment, the composition further includes an antimicrobial selected from consisting of glycerol monolaurate, lauric arginate, poly-lysine, and zinc lactate. Also provided are methods for treating bacterial vaginosis in a patient by intravaginally applying a treatment effective amount of subtilosin to the patient or a treatment effective amount of subtilosin and an antimicrobial selected from glycerol monolaurate, lauric arginate, poly-lysine, and zinc lactate to the patient. The present invention also relates to compositions that include an anti-microbial and/or spermicidal effective amount of subtilosin incorporated into a pharmaceutically acceptable aqueous solution, non-aqueous solution, nanofiber, hydrogel, gel, nanogel, suspension, ointment, jelly, insert, suppository, sponge, salve, cream, foam, foaming tablet, or douche. Subtilosin A (commonly referred to as subtilosin) is produced by both “Bacterial vaginosis prophylactic effective amount” is used herein to mean that amount which results in a sufficient concentration of subtilosin at a desired site to inhibit the development of bacterial vaginosis in a patient. “Treatment effective amount” is used herein to mean that amount which results in a sufficient concentration of subtilosin at an infected site to therapeutically ameliorate or reduce the effects of the disease. The disease being treated can be the first occurrence or a subsequent reoccurrence of the disease in the patient. “Anti-microbial effective amount” is used herein to mean that amount which results in a sufficient concentration of subtilosin to kill or inhibit the growth of one or more microorganisms (e.g. facultative and anaerobic microorganisms including but not limited to “Spermicidal effective amount” is used herein to mean that amount which results in a sufficient concentration of subtilosin to kill or disable sperm. The compositions used in the instant invention may be applied topically to prevent or treat bacterial vaginosis or kill or disable sperm. For topical administration, suitable carriers or vehicles include polar, protic solvents, such as, water or normal saline, non-polar solvents, lipids, ointments, jellies, inserts and foaming inserts (suppositories, sponges, and the like) salves, creams, foams, douches, nanofibers, hydrogels, gels, nanogels, or the like. The compositions may also be suspended in a suspension medium that is not miscible with water, for example, petrolatum, or may be formulated in an emulsion (water-in-oil or oil-in-water). More particularly, the compositions can be applied intravaginally for the prevention or treatment of bacterial vaginosis. The topical composition containing subtilosin could, for example, be applied with an applicator or an intravaginal device or the topical composition could be coated on a male or female condom or other sexual barrier devices, such as diaphragms, cervical caps, and the like. For topical applications, the pharmaceutically acceptable carrier may additionally comprise organic solvents, emulsifiers, gelling agents, moisturizers, stabilizers, surfactants, wetting agents, preservatives, time-release agents, and minor amounts of humectants, sequestering agents, dyes, perfumes, and other components commonly employed in pharmaceutical compositions for topical administration. Solid dosage forms for topical administration include suppositories, powders, and granules. In solid dosage forms, the compositions may be admixed with at least one inert diluent such as sucrose, lactose, or starch, and may additionally comprise lubricating agents, buffering agents and other components well known to those skilled in the art. The compositions of the invention may also be impregnated into absorptive substrate materials, such as sponges, or coated onto the surface of solid substrate materials, such as male or female condoms, diaphragms, cervical caps, or medical gloves, to deliver the compositions to vaginal or other potentially infectable epithelium. Other articles and delivery systems of this type will be readily apparent to those skilled in the art. A method of coating a condom with a composition comprising subtilosin comprises coating the whole surface or necessary portion of a condom by dropping, dipping, coating or spraying a solution containing subtilosin. Condom coating methods are well-known, and the subtilosin compositions can be incorporated into the known condom coating compositions, including lubricant compositions. Preferred coating compositions include silicon, which provides lubricity and releases the composition in a time-release manner. In this way, a condom having a spermicidal and/or anti-microbial effect and a lubricating effect can be obtained. Bioadhesive polymers may also be used to prolong the time-release aspects of the particular topical or other medicament employed. Subtilosin can also be impregnated into the condom during manufacture by processes known in the art. The amount of subtilosin applied on one condom can be any amount that provides the desired prophylactic effect with little or no side effects, preferably from about 0.001 mg to about 1000 mg. Coating a condom is carried out on one side or to both the inner surface and the outer one. In the present invention, subtilosin is generally administered in such a dosage as to achieve the desired actions with limited or no side effects. Although the actual dosage should be determined according to the judgment of doctors, the preferred concentration in a pharmaceutically acceptable carrier can vary from about 0.00005% to about 5% by weight. The following non-limiting examples set forth herein below illustrate certain aspects of the invention. An in situ forming hydrogel has two components, a polymer and a crosslinker. In When 50% of the arms have TP groups (as seen in The RGD sequence is known to preferentially bind to α,β-integrins. As a result, RGD adhesive nanocarriers should promote stronger contact between the hydrogel and the vaginal mucosal membrane. The synthesis of a water-soluble RGD-containing nanocarrier is shown. Using the synthetic scheme shown in Synthesis and characterization of 4-arm and 8-arm PEG-RGD nanocarriers RGDC peptide (100 mg, 0.0 mM) was dissolved in sodium phosphate buffer (8 ml, 0.1 M, pH, 7.4) containing 10% dimethylformamide (DMF), and 1,6-hexane-bis-vinyl sulfone (HBVS) (6 equiv., 356.4 mg) was added to it ( Four-arm or eight-arm PEG20kDa-thiol polymer (30 mg) was dissolved in sodium phosphate buffer (0.1 M, pH, 7.4) and the RGDC peptide modified with HBVS linker (3 equiv., 3.2 mg) was added to it. The reaction mixture was stirred at room temperature for 8 hrs ( Multiple copies of lactic acid were attached to 4-arm and 8-arm PEG20kDa-SH polymers, via degradable thioester bond. ( Hydrogels were prepared using degradable thioester crosslinks as follows: the 8-arm PEG-LA nanocarriers (4%, 6% and 8%; w/v) were mixed with varying amounts (4% to 16%) of 4-arm PEG20kDa-NHS crosslinker in sodium phosphate buffer (20 mM, pH 7.4) at room temperature, and the time of hydrogel formation was recorded. ( Rheological measurements were performed at 37° C. using a rheometer with parallel plate geometry (plate diameter: 20 mm, gap: 300 μm). PEG-LA hydrogels (4% and 6% w/v, 1:2) were allowed to form between the parallel plates at RT, before ramping the temperature up to 37° C. The elastic/storage modulus G′ and viscous/loss modulus G″ of the hydrogels were measured as a function of strain and frequency using dynamic oscillatory tests. First, a strain sweep test was performed at a constant frequency of 1 Hz, in order to determine the linear viscoelastic regime. Next, a frequency sweep test (0.1-1 Hz) was carried out at a constant strain of 1%. All rheological measurements were done in triplicate and the mean±SEM reported. It was found that G′ was higher than G″ over the frequency range tested, indicating that the hydrogels were more elastic than viscous ( Based on these results for PEG-LA hydrogels, the feasibility of crosslinking nanocarriers with other functionalities to form a hydrogel is demonstrated. It is expected that the hydrogels will possess the physical attributes of a good barrier membrane: they are highly dispersible providing extensive coverage of irregular surfaces; they possess sufficient viscosity to slow viral diffusion; and have outstanding elastic properties to withstand applied strain allowing the hydrogel barrier to remain intact during physical activity. Preparation of Hydrogels with Passively Entrapped Lactic Acid. Eight-arm PEG-SH (4%, 6% and 20%; w/v) with 200 μg of lactic acid and either 4-arm PEG20kDa-NHS (8% and 12%: w/v) or 8-arm PEG20kDa-NHS (20% w/v) were mixed in PB at room temperature. The time of formation of these hydrogels is provided in the table below. The 8-arm PEG-LA nanocarriers (1 mg/100 μl) were dissolved in sodium phosphate buffer (20 mM, pH 7.4). Dissolved 8-arm PEG-LA, PEG-LA hydrogel, and hydrogel with passively entrapped lactic acid was dialyzed against 3.6 ml PBS (10 mM, pH 7.4) or acetate buffer (pH 4.3) at 37° C. Aliquots (1 ml) were withdrawn at pre-determined time-intervals and the medium was replenished. A lactate assay kit (BioVision, Inc.) was used for quantifying the amount of lactic acid released, as per the manufacturer's protocol (O.D. at 570 nm). ( Hydrogels were weighed (W0) and immersed in PBS (1.0 mL, 10 mM, pH 7.4) or acetate buffer (pH 4.3), and incubated at 37° C. The buffer was withdrawn at pre-determined time intervals and hydrogel weights were recorded (Wt). The swelling ratios were calculated as Wt/W0×100, and plotted against time. ( Hydrogels were weighed (W0) and immersed in PBS (1.0 mL, 10 mM, pH 7.4) or acetate buffer (pH 4.3), and incubated at 37° C. The buffer was withdrawn at pre-determined time intervals and hydrogel weights were recorded (Wt). The swelling ratios were calculated as Wt/W0×100, and plotted against time. ( The feasibility of producing stably aggregated PEG nanogel particles was determined. PEG nanogels (˜20 nm) were made using a one step synthetic procedure. As shown in Subtilosin A: a Safe Microbicidal Protein from The antimicrobial activity of subtilosin against Several microbicides under clinical development for the prevention of sexually transmitted infections (including those for which trials have recently been halted) have contraceptive properties (e.g., Pro2000, SAVVY, VivaGel, cellulose sulfate). However, none of those in development are spermicidal. Their contraceptive effects are mediated by effects on sperm function rather than cell death. While contraceptive activity in some cases is quite good (e.g., cellulose sulfate), it depends on the correct timing and placement of the product. A contraceptive microbicide that is truly spermicidal would not be as dependent on these variables, and would likely be more efficacious. We tested the effect of subtilosin on human sperm motility and the results are encouraging. This study was carried out by exposing whole semen to different concentrations of subtilosin. Thirty seconds after adding the compound to the semen, each sample was microscopically examined for sperm motility and forward progression. The subtilosin solution decreased the proportion of motile spermatozoa in a dose-dependent manner ( Subtilosin Produced by Cell-free supernatant (CFS) harvested from MRS broths was incubated for 48 hours at 37° C. in 5% CO2atmosphere (until approximately 106 CFU ml-1). Cells were removed from the culture by centrifugation (Hermle Z400K, LabNet, Woodbridge, N.J.) for 25 min at 4500×g and 4° C. Supernatants were filter-sterilized using 0.45 pin microfilters (Fisher, Pittsburgh, Pa.). Well diffusion inhibition assays were conducted as described by Cintas, L. M., et al., “Isolation and characterization of pediocin L50, a new bacteriocin from Lactic acid concentrations in the CFS were determined using a D-Lactic acid/L-Lactic acid test kit and according to the manufacturer's protocol (Roche Boehringer, Mannheim, Germany). After completing the steps of the protocol, the gathered data was applied to the provided equations in order to accurately calculate the quantities of each acid form in the sample. The CFS was exposed to seven different enzymes (Sigma; SDS-PAGE was conducted using a Tris-Tricine gel made in a Bio-Rad casting apparatus (Bio-Rad, Hercules, Calif.). The gels were loaded with either 20 μl of marker or 200 μl of sample [1:1 sample+loading buffer (Bio-Rad)]. Nisin (106IU g−1, 2 mg ml−1) was used as the positive control. The procedure was conducted in 0.2 mol l−1Tris-base anode running buffer (pH=8.9) and 0.1 mol l−1Tris/0.1 mol l−1Tricine/0.1% SDS cathode running buffer (pH=8.25) in a Mini-Protean 3 (Bio-Rad) chamber with Power-Pac 300 power source (Bio-Rad). Upon completion of electrophoresis, the gel was cut into identical halves; one half was treated for the overlay process while the other was used in the staining procedure. The overlay gel was fixed for 2 h in 100 ml of 10% acetic acid/20% isopropanol buffer, rinsed 3 times over 2 h in 100 ml ddH2O, and stored overnight in ddH2O at 4° C. (all steps occurred under rotation). The following day, it was laid onto a dried enriched TSA plate and overlaid with Using a stock overnight culture, Further purification of the 30% ammonium sulfate precipitate was achieved with Sep-Pak® Light C18 Cartridges (Waters, Milford, Mass.) to separate the protein of interest based on an assumed hydrophobic nature. In each instance, 0.5 ml of liquid was passed through the column at a flow rate of 0.2 ml min−1. The cartridge was initially rinsed with 0.5 ml 100% methanol and equilibrated by four 0.5 ml washes with ddH2O to remove any traces of the methanol. Following the water washes, the sample was loaded onto the cartridge and the flow-through was collected. This was followed by another four 0.5 ml washes with ddH2O, with each fraction collected individually. immediately after the water washes, the column was washed sequentially with 1 ml of 50%, 70%, 90% and 100% methanol, and individual 0.5 ml fractions were collected. Antimicrobial activity was confirmed by the well diffusion assay. The ability of the compound to retain activity under elevated temperatures was tested by incubating the sample at a given temperature for 0-60 min. After each time point 200 μl was aliquoted and used to create 2-fold serial dilutions in ddH2O. Each dilution was used in a well diffusion assay; the reciprocal value of the lowest dilution that maintained activity is considered the protein concentration in arbitrary units (AU) ml−1. The level of antimicrobial activity of the sample was tested at varying pH levels. The pH of the solution was adjusted to fall within the range of 2-10 using either 3 mol l−1HCl or NaOH. The samples were incubated at room temperature for 1 min before conducting a well diffusion assay against DNA was extracted from overnight cultures of Polymerase chain reactions (PCRs) were performed to assess the relatedness between the bacteriocin produced by While the Yogu Farm™ beverage was purported to contain The CFS of a Using equations provided by the manufacturer's protocol, it was determined that Inhibition assays revealed that activity was completely lost in the presence of pepsin and proteinase K, and significantly decreased by trypsin and chymotrypsin, confirming the proteinaceous nature of the compound ( The protein was fully precipitated out of solution at 30% ammonium sulfate concentration, and the presence of the bacteriocin was confirmed on SDS-PAGE gels with a large zone of inhibition in the overlay portion corresponding to the known size of subtilosin (data not shown). Inhibition assays indicated that the protein was solely and completely eluted from the columns by 90% methanol. They also confirmed activity was wholly due to the antimicrobial peptide and not background activity from the methanol. PCR analysis showed Stock cultures of The partially purified preparation of subtilosin was prepared as described in Sutyak et al., “Isolation of the The effect of subtilosin on ATP depletion in The total ATP concentration in The ability of subtilosin to affect the transmembrane electric potential (ΔΨ) of Briefly, The ability of subtilosin to affect the transmembrane pH gradient (ΔpH) of Initially, Subtilosin Causes an Efflux of ATP from The effect of subtilosin on intracellular ATP levels in The ability of subtilosin to dissipate the transmembrane electrical potential (ΔΨ) in Cells were energized with 2.2 mM glucose at start of fluorescence readings. Two μmol/L valinomycin (Val) was used to transform the ΔΨ of the PMF into ΔpH Addition of subtilosin caused an instant drop in the signal intensity of the pH dependent, fluorescent probe BCECF-AM, indicating an immediate intracellular decrease in pH in the The results show that subtilosin acts by fully depleting the transmembrane pH gradient (ΔpH) and causing an immediate efflux of intracellular ATP, but has no effect on the transmembrane electric potential (ΔΨ). The current results strongly suggest that the changes in the PMF brought about by subtilosin are due to the formation of transient pores in the cytoplasmic membrane of Subtilosin was prepared as previously described in Sutyak et al., “Isolation of the The concentration of subtilosin in the column-purified fraction was determined using the Micro BCA Protein Assay Kit according to the manufacturer's protocol (Pierce, Rockford, Ill., USA). In brief, the assay measures the reduction of Cu2+ to Cu1+ by colorimetric detection of Cu1+ by bicinchoninic acid. Bovine serum albumin (BSA) was used to develop a standard curve with concentrations ranging from 0.5 to 20 μg/mL; the concentration of subtilosin was calculated using the R value from the trendline of the standard curve graph. The concentration of subtilosin in the CFS was not measurable with the Micro BCA Protein Assay due to the high level of background proteins in the solvent (MRS medium). As an alternative, the protein concentration was calculated by comparing the antimicrobial activity of known concentrations of column-purified protein to equal volumes of CFS. Five two-fold dilutions were made from the stock samples of both the CFS and the column-purified fraction. Well diffusion assays were performed using 50 μL of each dilution against As reported previously, the concentration of lactic acid in the CFS was measured to assess its potential effects on antimicrobial activity and cell viability. Sutyak et al., “Isolation of the The EpiVaginal (VEC-100) ectocervical tissue model (MatTek Corporation, Ashland, Mass., USA) was used and maintained as fully described by Dover et al., “Safety study of an antimicrobial peptide lactocin 160, produced by the vaginal Following the designated exposure times, the MTT (3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay was used to determine overall cell viability. The data were used to approximate an effective time (ET) that would reduce cell viability to 50% (ET-50). The MIT assay was carried out according to the protocol outlined by Dover et al. Briefly, the viability of ectocervical cells after exposure to subtilosin was measured as a direct proportion of the breakdown of the yellow compound tetrazolium to the purple compound formazan, since only living cells can cause this reaction to occur. Tissues were exposed to subtilosin and the two controls for several designated time points; at the conclusion of each, the liquid in the plate wells was combined with the liquid from the tissue inserts. This mixture was then assayed spectrophotometrically using a 96 well-plate reader (MRX revelation, Dynex Technologies, Va., USA) to determine the level of tetrazolium degradation. The viability (%) of the treated tissue inserts was calculated according to an equation provided by the manufacturer: % viability=OD570(treated tissue)/OD570(negative control tissue). The exposure time that reduced tissue viability by 50% (ET-50) was calculated according to [V=a+bxlog(t)] described by Ayehunie et al., “Organotypic human vaginal-ectocervical tissue model for irritation studies of spermicides, microbicides, and feminine-care products,” Toxicology in Vitro 20(5):689-98 (2006), where V=% viability, t=time in minutes, and “a” and “b” are constants representing the viability data from the time points preceding and following 50% viability. On the whole, there is a direct relationship between the length of the ET-50 and the toxicity of the tested application (i.e., a shorter ET-50 corresponds to a more harmful compound). The CFS gathered from a Two semen samples were collected on the day of experimentation. Each sample was collected by self-masturbation in a polypropylene specimen container (Fisher) prior to transport to the laboratory. Within 1 hour of collection, the samples were pooled. Total sperm count was calculated using bright field light microscopy (Olympus BX50; 400×) after dilution (1:50) of the semen in normal saline. The initial percentage of motile sperm was calculated prior to testing with a neubauer hemacytometer. The determination of motile sperm % was made using randomly Selected field views (400×) from a count of between 104-201 cells. Any visibly moving spermatozoa (directional or stationary) were counted as motile cells. The percentage of forward progressing spermatozoa was subjectively determined based on the assumption that 70% of the sperm in a normal sample would behave in such a manner. The samples used in this experimentation fell into such a “normal” category. Treatment of Spermatozoa with Subtilosin A modified Sander-Cramer test was used to determine the effect of column-purified subtilosin on human spermatozoa motility. This measured the effect of subtilosin after 30-second exposure times of 5 volumes (200 μL) of the solution at each dilution (25% and 50% in normal saline, and 100%) with one volume (40 μL) of whole semen. The motilities of cells from random high-magnification fields (400×) of the sample were determined in duplicate as described above. The % motility data were arcsine transformed prior to further examination. StatMost32 (version 4.1) statistical software (DataMost Corporation, Sandy, Utah, USA) was used to calculate all statistical parameters. The % values of motility were presented as averages and 90% confidence limits. Any differences between treatment groups were assessed by the Newman-Keuls multiple range test. Differences were deemed significant at the 0.05 level of confidence. The concentration of subtilosin in the column-purified sample was estimated at 135.7 μg/mL. The CFS and column-purified sample produced identical zones of inhibition at each dilution (data not shown); therefore, the concentrations of protein in both solutions were assumed to be equivalent. While it is improbable that a 100% yield would be attained from column chromatography, previous work has shown that protein concentrations can be precisely calculated based on the comparisons we conducted. Due to the difficulty in measuring the CFS protein concentration via other assays, the chosen method was deemed the most accurate and reproducible. After 48 hours of exposure to subtilosin, the Epi Vaginal ectocervical tissues retained a high level of viability compared to the positive control, Nonoxynol-9, and the negative control, miconazole nitrate ( Subtilosin reduces human sperm motility in a dose-dependent manner ( Similar to motility, forward progression of spermatozoa is reduced in a dose-dependent fashion by subtilosin. In control samples, 70% of sperm exhibited forward progression; in the presence of 50 μL subtilosin this decreased to 50-70%, while 100 μL caused a decline to only 10% forward progression. All forward progression was eliminated after treatment with 200 μL subtilosin, with most sperm tails becoming coiled. Subtilosin was found to significantly reduce the motility of human spermatozoa in a concentration-dependent manner for all concentrations tested. The effect of subtilosin on the forward progression of spermatozoa was also observed to be a dose-dependent interaction. Serial dilutions showed a steady decline in forward progression, with all progression halted at the highest concentration tested. It was also noted that at the highest concentration, the tails of the sperm cells were curved or coiled, indicating the cells were damaged beyond a simple restriction of movement. Coiling of the cells is considered to be a sperm abnormality, and may indicate damage to the plasma membrane. Tail coiling has been observed after in vitro exposure of monkey spermatozoa to methyl mercury. Subtilosin in Combination with Other Natural Antimicrobials The partially purified preparation of subtilosin was prepared as described above. Sterile Lauricidin® (glycerol monolaurate) was a gift from Dr. Alla Aroutcheva of Rush Medical Center, Chicago, Ill. A 2 mg/mL stock Solution of glycerol monolaurate was prepared in BHI+3% horse serum broth pre-warmed to 37° C. MIRENAT-CF was a gift from Vedeqsa Corp. (Barcelona, Spain), and contained 1 mg/mL lauric arginate (Nα-lauroyl-L-arginine ethyl ester monohydrochloride, LAE). A stock solution containing 25% ε-poly-L-lysine (250 mg/mL) was a gift from Chisso America, Inc. (Lot #2090501; Rye, N.Y.). A solid stock supply of zinc lactate (Puramex Zn) was a gift from Purac America, Inc. (Lot #0807000376; Lincolnshire, Ill.). A 5.45 mg/mL stock solution of zinc lactate was made using ddH2O. All antimicrobial solutions were filter-sterilized using a 0.45 μm filter (Nalgene, Rochester, N.Y.) prior to use. The ability of each antimicrobial to individually inhibit The interaction between subtilosin and the chosen antimicrobials was tested via a “checkerboard” assay that allowed for testing of multiple antimicrobials at various concentrations at the same time. The assays were performed according to Badaoui Najjar, et al., “Epsilon-poly-L-lysine and nisin A act synergistically against Gram-positive food-borne pathogens The kinetic growth curve data from all assays was analyzed using Microsoft Excel 2007 (Microsoft, Redmond, Wash.). Isobolograms were created for each synergy assay as a way to visualize the presence of synergy, additive effect, or antagonism. In an isobologram, the x- and y-axes represent the concentrations of each antimicrobial; the MIC of each substance is then plotted on the graph, and the two points are joined by a line. The mixed concentrations of antimicrobials that caused complete inhibition of microbial growth are then plotted on the graph. Points that fall below the line indicate synergy, points on the line show an additive effect, and points above the line demonstrate antagonism. (Chou, T.-C., “Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies,” Pharmacol Rev. 58: 621-81 (2006)). The MIC of subtilosin, GML, LAE, poly-lysine, and zinc lactate against G. vagina/is was tested by the broth microdilution method in BHI broth supplemented with 3% horse serum. As seen in Once the individual MICs of all the chosen compounds were calculated, a checkerboard assay was performed using subtilosin in combination with one other substance. Each assay was designed to test a wide range of concentrations, beginning with one slightly above that of each compound's individual MIC and decreasing in a serial manner to a zero concentration (negative control). Combinations of concentrations below each of the MIC levels that caused complete inhibition of microbial growth were analyzed with isobolograms to determine the presence of synergy, additive effect, or antagonism. Since GML has demonstrated antimicrobial activity against the BV-associated pathogen The second natural antimicrobial, lauric arginate, has previously been shown to synergize with the An isobologram was constructed using the individual MICs of subtilosin and poly-lysine ( An isobologram was constructed using the individual. MICs of subtilosin and zinc lactate ( The antimicrobial activity of subtilosin and four natural antimicrobials were investigated alone and in combination against the BV-associated pathogen A multifunctional polyethylene glycol-based hydrogel that includes a multi-arm polyethylene glycol cross-linking unit covalently bound to at least four multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit includes an agent coupled to the nanocarrier unit and each agent is selected from pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding, provided that each nanocarrier unit comprises a different agent. 1. A multifunctional polyethylene glycol-based hydrogel comprising a multi-arm polyethylene glycol cross-linking unit covalently bound to at least four multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit comprises an agent coupled to the nanocarrier unit and each agent is selected from the group consisting of pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding, provided that each nanocarrier unit comprises a different agent. 2. The hydrogel of 3. The hydrogel of 4. The hydrogel of 5. The hydrogel of 6. The hydrogel of 7. The hydrogel of 8. The hydrogel of 9. The hydrogel of 10. The hydrogel of 11. The hydrogel of 12. A method for preparing the hydrogel of 13. The method of 14. A kit for use in preparing a multifunctional polyalkylene oxide-based hydrogel, said kit comprising:
(a) an amount of multi-arm polyethylene glycol cross-linking units comprising a thiol-reactive functional group coupled to each arm; and (b) an amount of multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit comprises a thiol group coupled to half of the arms and an agent coupled to the remaining arms of each nanocarrier unit and each agent is selected from the group consisting of pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding; wherein said amounts of the cross-linking units and the nanocarrier units are sufficient to produce a hydrogel when combined. 15. A method for prophylactically reducing the risk of development of HIV in a patient comprising intravaginally or intrarectally administering to a patient:
(a) an amount of multi-arm polyethylene glycol cross-linking units comprising a thiol-reactive functional group coupled to each arm; and (b) an amount of multi-arm polyethylene glycol nanocarrier units, wherein each nanocarrier unit comprises a thiol group coupled to half of the arms and an agent coupled to the remaining arms of each nanocarrier unit and each agent is selected from the group consisting of pH-lowering agents, bioadhesion agents, microbicidal-spermicidal agents, and agents that inhibit free and cell-associated HIV binding; wherein said amounts of the cross-linking units and the nanocarrier units are sufficient to produce a hydrogel when combined. 16. An article comprising the hydrogel of 17. A topical composition comprising an anti-microbial and/or spermicidal effective amount of subtilosin incorporated into a pharmaceutically acceptable aqueous solution, non-aqueous solution, nanofiber, hydrogel, gel, nanogel, suspension, ointment, jelly, insert, suppository, sponge, salve, cream, foam, foaming tablet, or douche. CROSS-REFERENCE TO RELATED APPLICATIONS
STATEMENT REGARDING FEDERALLY SPONSORED RESEARCH
BACKGROUND OF THE INVENTION
SUMMARY OF THE INVENTION
BRIEF DESCRIPTION OF THE DRAWINGS
DETAILED DESCRIPTION OF THE INVENTION
EXAMPLES
Characteristics of Nonfunctionalized Hydrogels
Adhesive RGD Nanocarriers for Greater Mucosal Hydrogel Retention and Prevention of HIV Binding.
Synthetic Feasibility of Preparing the RGD Nanocarrier Crosslinker is Demonstrated.
Synthesis and Characterization of 4-Arm and 8-Arm PEG-LA Nanocarriers.
Synthesis and Characterization of PEG-LA Nanocarrier-Based Hydrogels.
Time of formation of hydrogels with passively entrapped lactic acid; Mean ± S.D., n = 3 8-arm 4-arm Time of hydrogel PEG20 kDa-SH (mg) PEG20 kDa-NHS (mg) formation (min) 4 8 9.8 ± 0.2 6 12 6.6 ± 0.2 20 20 1.67 ± 0.1
Release of Lactic Acid from PEG-LA Nanocarriers, PEG-LA Nanocarrier-Based Hydrogels, and Hydrogels with Passively Entrapped Lactic Acid.
Hydrogel Swelling and Degradation Studies.
Hydrogel Swelling and Degradation Studies.
Polyanionic Stably Aggregated Nanoparticles to Bind HIV Virions.
Subtilosin A: Spermicidal Microbicide.
Bacterial Strains, Growth Conditions, and Culture Media
Sample Preparation
Assay of Antimicrobial Activity
Determination of Lactic Acid Concentrations
Enzymatic Digestion to Confirm Proteinaceous Nature of Antimicrobial Compound
Protein Visualization
Protein Purification
Effect of Temperature and pH on Antimicrobial Activity
Genetic Analysis
Characterization of Unknown Isolate
Range of Antimicrobial Activity
Determination of Lactic Acid Concentrations
Effect of Enzyme Digestion, Temperature and pH on Antimicrobial Activity
Protein Purification
Genetic Analysis
Analysis of Anti-Microbial Activity
Bacterial Strains and Growth Conditions.
Preparation of Antimicrobial Solutions.
ATP Efflux Assay.
Effect of Subtilosin on Proton Motive Force (PMF) in
ΔΨ Dissipation Assay.
ΔpH Dissipation Assay.
Subtilosin has No Effect on
Subtilosin Causes an Immediate Depletion of the Transmembrane pH Gradient (ΔpH).
Analysis of Spermicidal Activity
Production of Subtilosin
Determination of Protein Concentration
Determination of the Presence of Weak Organic Acids
EpiVaginal Ectocervical Tissue Model
MTT Viability Assay
Semen Sample Collection and Analysis
Data Analysis
Determination of Protein Concentration
Cell Viability % and ET-50 Values
Quantitative Observations of Motile Spermatozoa
Semiquantitative Observations of Spermatozoa: Forward Progression
Bacterial Strains and Growth Conditions
Determination of Minimal Inhibitory Concentrations (MICs)
Checkerboard Assay
Graphical Presentation of the Data
Determination of MICs
Determination of Synergy Between Antimicrobial Substances
Interaction Between Subtilosin and Glycerol Monolaurate (GML)
Interaction Between Subtilosin and Lauric Arginate (LAE)
Interaction Between Subtilosin and ε-Poly-L-Lysine
Interaction Between Subtilosin and Zinc Lactate
Discussion